patellar tendonitis recovery time
:max_bytes(150000):strip_icc()/treatment-of-a-patellar-tendon-tear-25495911-5c77359a46e0fb0001d83ca7.png) Patellar Tendon Tear Causes, Diagnosis, and Treatment
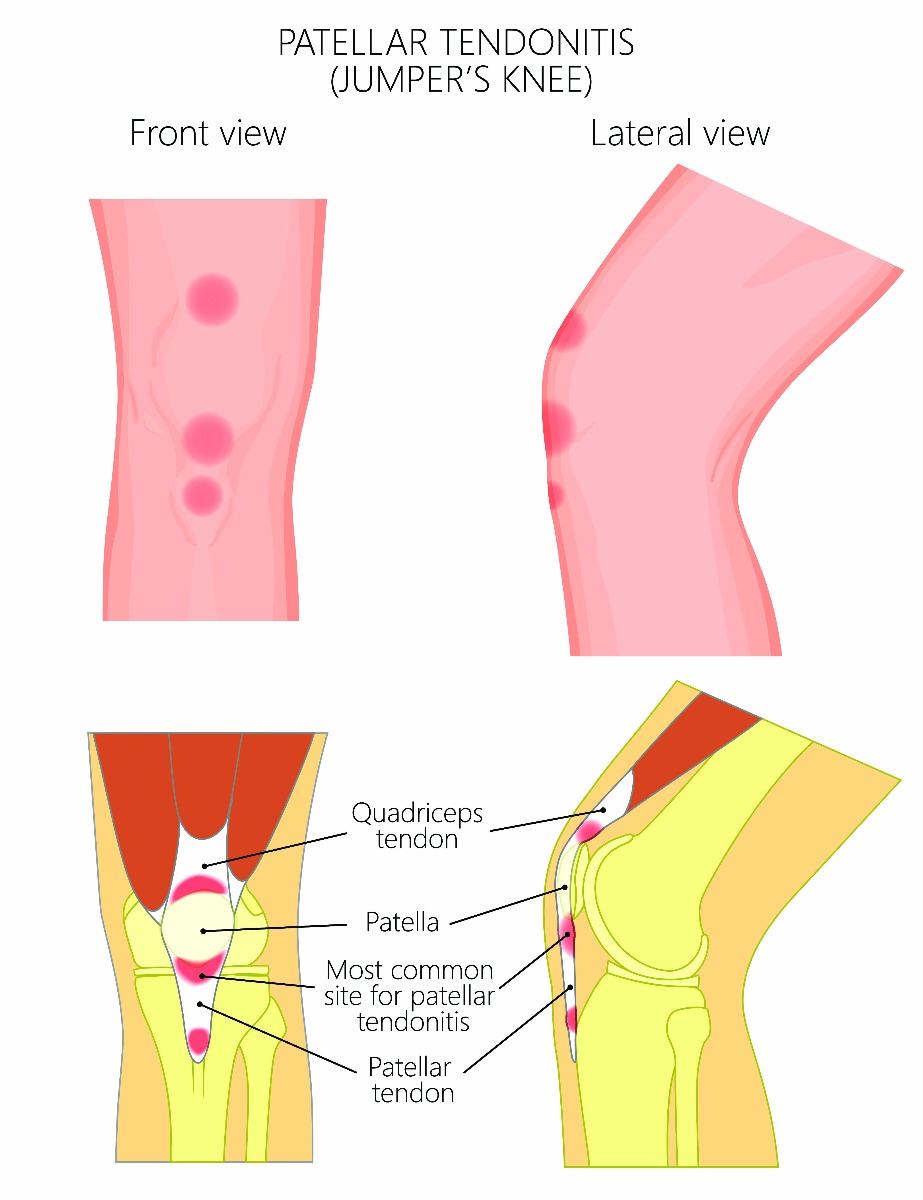
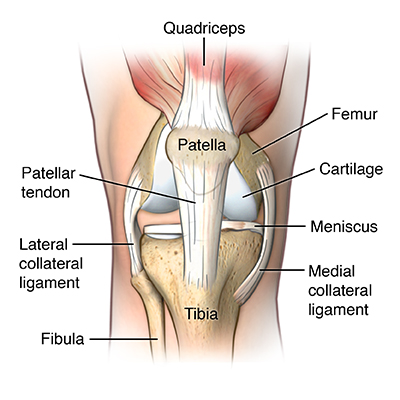
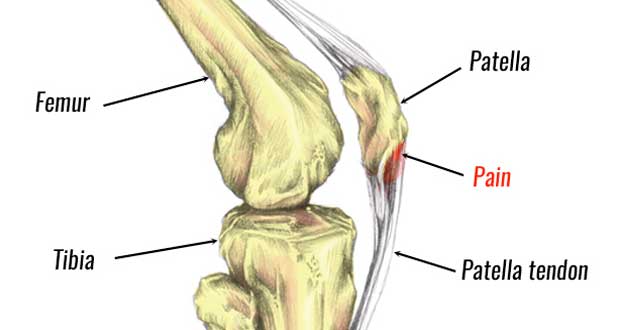
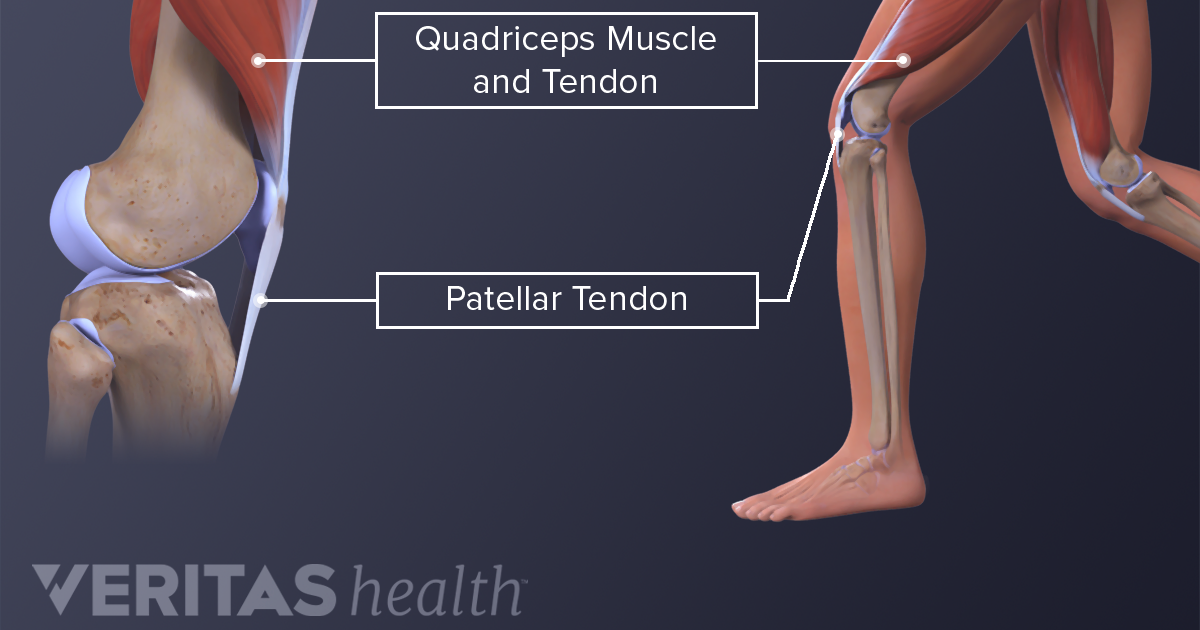
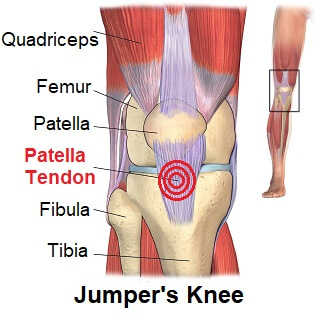
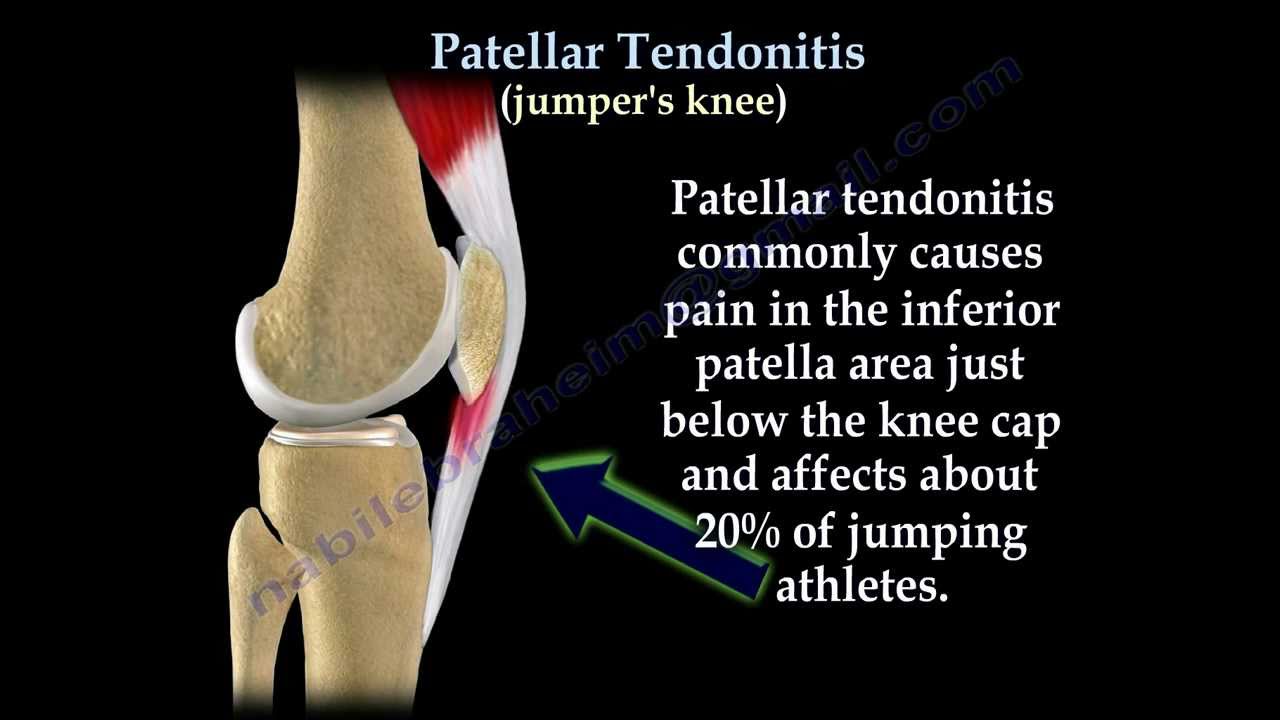
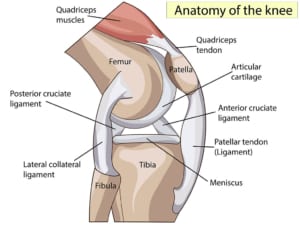
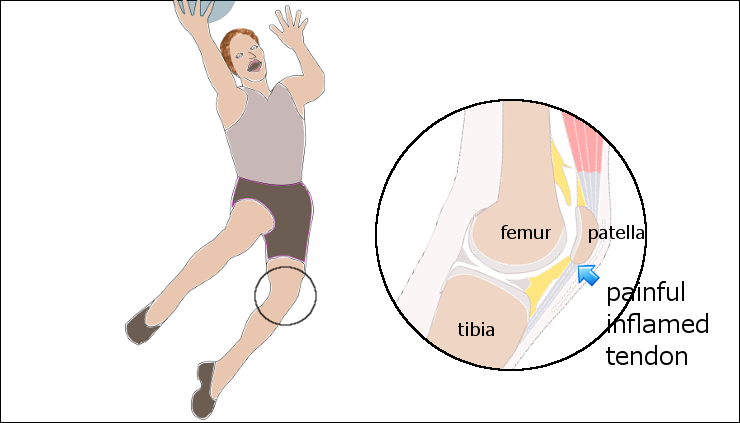
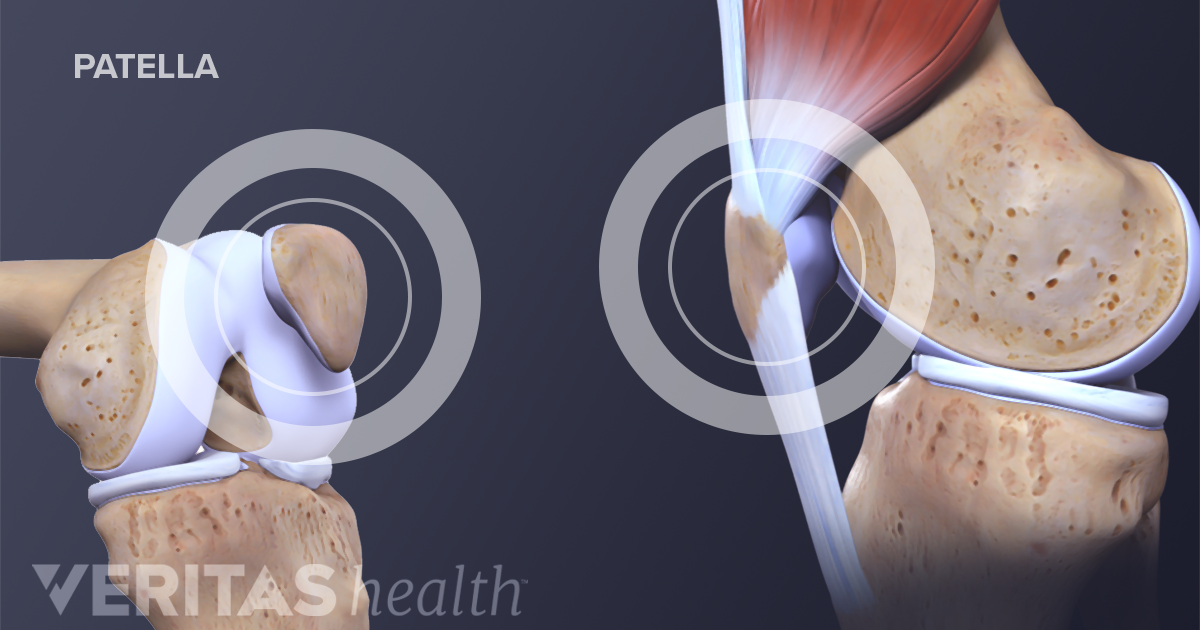
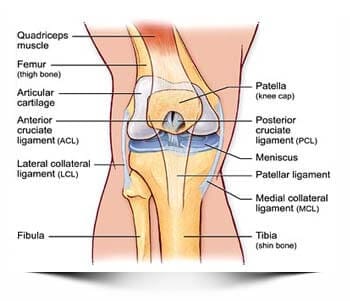
Patellar Tendon Tear Causes, Diagnosis, and TreatmentPatient's Guide to Patellar TendonitisIntroductionThe problems of alignment or overuse of the knee structures may cause tension, irritation, and/or injury. This causes pain, weakness and swelling of the knee joint Patellar tendonitis (also known as the jumper's knee) is a common condition of overuse associated with running, repeat jumping and landing, and kicking. This guide will help you understand Anatomy What parts of the knee are involved? The patella (kneecap) is the bone moved in the front of the knee. This unique bone is wrapped within a tendon that connects large muscles in the front of the thigh, quadruple muscles, with the lower leg of the warm leg. The lightening of the quadruple muscles places a shrimp in the quadruple mechanism tendons. This action makes the knee straight. The patella acts as a fulcrum to increase the strength of the quadruple muscles. The long bones of the femur and the tibia act as lever arms, placing strength or load in the joint of the knee and surrounding soft tissues. The load amount can be quite significant. For example, the joint reaction forces of the lower limb (including the knee) are two or three times the body weight during the walk and up to five to seven times the body weight when running. Related document: Causes What causes this problem? Patelar tendonitis occurs more often as a result of tensions placed in the knee support structures. Running, jumping, and repetitive reflection of the knee in the extension (for example, by rising from a deep squadron) contribute to this condition. The excess-use injuries of sports activities are the most common cause, but anyone can be affected, even those who do not participate in sports or recreational activities. There are extrinsic (outside) factors that are linked to lesions tendons of excessive use of the knee. These include inappropriate footwear, training errors (frequency, intensity, duration) and surface or soil (hard surface, cement) that are used for sport or event (such as running). Training errors are summed up by the "all" rule. This refers to training too, too far, too fast, or too long. Advancing the training program too fast is an important cause of patellar tendonitis. Important intrinsic (internal) factors such as age, flexibility and joint laxity are also important. The poorness of the foot, ankle and leg can play a key role in tendonitis. Flat standing position, patella tracking alterations, tibia rotation called tibial torsion, and a leg length difference can create an increased and often uneven load in the quadriceps mechanism. Any muscle imbalance of the lower limb (from the hip to the fingers) can affect the quadruple muscle and affect the joint. Individuals who are overweight may have added problems with the load and muscle imbalance that lead to patellar tendonitis. The strength of the patellar tendon is in direct proportion to the number, size and orientation of the collagen fibers that make up the tendon. Excessive use is simply a misalignment between the load or stress on the tendon and the ability of that tendon to distribute the force. If the forces placed on the tendon are greater than the strength of the structure, then injury may occur. Repeated microtrauma in muscle union tendon can overcome the ability of the tendon to heal. The breakdown of tissues occurs by triggering an answer that leads to tendonosis. Chronic tendonitis is really a problem called tendonosis. The swelling is not present. Instead, the degeneration and/or scarring of the tendon has developed. Chronic tendon injuries are much more common in athletes (30 to 50 years old). SymptomsHow does the condition feel? The pain of patellar tendonitis feels right under the bottle. Pain is more noticeable when you move your knee or try to kneel. The more the knee moves, the more tender it develops in the area of the attachment of the tendon under the knee. Diagnosis How does Dr. Kiritsis diagnose the problem? The diagnosis begins with a complete history of your knee problem followed by a knee exam, including the patella. There is usually tenderness with palpation of the inflated tissues in insertion of the tendon into the bone. The knee will be evaluated for the range of movement, strength, flexibility and joint stability. Dr. Kiritsis will look for intrinsic and extrinsic factors that affect the knee (especially sudden changes in training habits). Potential problems are identified with a lower alignment of the limb. Dr. Kiritsis will also check the hamlets and hips for narrative weakness and rigidity. X-rays can be ordered on the initial visit to your doctor. An X-ray can show fractures of the tibia or the patella but X-rays do not show lesions of soft tissue. In these cases, other tests may be suggested, such as ultrasound or magnetic resonance imaging (MRI). Ultrasound uses sound waves to detect tendon tears. Magnetic resonances use magnetic waves instead of x-rays to show the body's soft tissues. This machine creates images that look like slices of the knee. This test is usually done to look for injuries, such as tears in the quadriceps. This test does not require special needles or dye and is painless. Treatment What treatment options are available? Non-surgical treatment The initial treatment for acute patellar tendonitis begins by decreasing inflammation in the knee. Dr. Kiritsis may suggest relative rest and anti-inflammatory drugs, such as ibuprofen, especially when the problem comes from overuse. Acetaminophen (Tylenol) can be used for pain control if anti-inflammatory medications cannot be taken for any reason. Relative rest is a term used to describe a recovery-rest process based on the severity of symptoms. Rest pain means strict rest and a short time of immobilization in a spine or bracelet is necessary. When the pain is no longer present at rest, then a gradual increase in the activity is allowed while the rest pain does not return. Physical therapy can help in early stages by reducing pain and inflammation. Your physical therapist may use ice massage, electrical and ultrasound stimulation to limit pain and control (but not completely prevent) inflammation. An amount of inflammatory response is needed for a good healing response. The therapist will prescribe stretching and strengthening exercises to correct any muscle imbalance. Excentric muscle strength training helps prevent and treat injuries that occur when high tensions are placed on the tendon during closed kinetic chain activities. Excentric contractions occur while the contracted muscle elongates. Closed kinetic chain activities means that the foot is planted on the ground while the knee bends or straightens. Researchers have also discovered that patellar tendonitis responds to a concentric-eccentric program of exercises for the previous tibialis muscle. The anterior tibialis muscle is found along the front of the lower leg. It is the muscle that helps you to dorsiflex the ankle (pulling your toes and ankle to the face). Flexibility exercises are often designed for the muscles of the thigh and the calf. Specific exercises are used to maximize the control and strength of quadruple muscles. You will be shown how to ease the jump or the performance of sports using good training techniques. Strength training outside the leg season, particularly quadruple muscles is recommended. Bronze or tap of the patella can help you do exercises and activities with less pain. The majority of the devices for paellofemoral problems are made of soft fabric, such as fabric or neoprene. You slide them over your knee like a sleeve. A small buttock on the side of the patella to keep it lined inside the femur slot. An alternative to the bra is to record the patella instead. The therapist applies and adjusts the ribbon on the knee to help realign the patella. The idea is that when you hold or press the knee, the bottle stays in better alignment within the femoral slot. This in turn is intended to improve the spin of the quadriceps muscle so that the patella stays aligned in the slot. Patients report less pain and better functioning with these forms of treatment. Prevention of future injuries through patient education is a key component of the treatment programme. This is true if conservative care or surgical intervention is required. It is essential to modify intrinsic and extrinsic risk factors. Coaches, coaches and therapists can work together to design a training program that allows you to continue training without irritating the tendon and surrounding tissues. Remember to warm up and stretch before exercise. Some experts recommend cooling and stretching after exercise as well. Know your limits and don't overpower it. Use ice after activity if indicated by pain or swelling. The coating should be limited to no more than 20 minutes to avoid reflexive vasodilation (increasing circulation to the area to rinse it causing greater inflammation). Heat can be used in cases of chronic tendinosis to stimulate blood circulation and promote tissue healing. Whenever you have to lose exercise for any reason or when we train for a specific event, adjust your training program accordingly. Avoid the "too much" training errors mentioned above. Injections such as Toradol and Platelet Rich Plasma (PRP) can be an option and will be reviewed with you by Dr. Kiritsis. Surgery Surgery is rarely necessary when a wide range of protective measures, relative rest, ice, support and rehabilitation are used. If non-surgical treatment does not improve your condition, surgery may be suggested. Surgery is designed to stimulate healing through revascularization (reparation of blood supply). The weak and damaged tissue is removed and the injured tendon is repaired. The remodeling of tissues by surgery can restore the function. The arthroscopic procedures can normally be performed on an outpatient basis. This means you can leave the hospital the same day. Rehabilitation What should I expect while I recovered? Non-surgical rehabilitation Patellar tendonitis is usually self-limiting. That means that the condition will resolve with rest, activity modification and physical therapy. The repetition of the problem is common for patients who do not allow the patellar tendon to recover completely before resuming the formation or other aggravating activities. Physical therapy for approximately four to six weeks is usually recommended. The goal of treatment is to calm pain and inflammation, correct muscle imbalances and improve the function of the quadruple mechanism. With a well-planned rehabilitation program, most patients can return to their previous level of activity without recurrent symptoms. After SurgeryDr. Kiritsis will have your patients participate in formal physical therapy after knee surgery. More surgeries involved in patellar readjustment or restorative procedures for tendon tissue require a delay before going to therapy. And rehabilitation can be slower to allow the tendon to heal before too much tension can be put on the knee. The first few physiological treatments are designed to help control the pain and inflammation of the surgery. The physical therapist will choose exercises to help improve the movement of the knee and to get the toned and active quadruple muscles back. Muscle stimulation, using electrodes on the quadruple muscle, may first be needed for the muscle to move again. As the program evolves, more challenging exercises are chosen to safely advance the strength and function of the knee. The key is to get soft tissues to balance through safe stretching and gradual strengthening. The goal of the physical therapist is to help you keep your pain under control, ensure that you place only a safe amount of weight on the healing knee, and improve your strength and range of motion. When you're okay, regular visits to the therapist's office will end. The therapist will remain a resource, but you will be in charge of doing your exercises as part of an ongoing startup program. OrthoVirginia, is dedicated to providing you with a pleasant visit. Call with any questions or make an appointment. Orthopedic surgery treatments by PBHS © 2021 •

How Long Does Patellar Tendonitis Take To Heal?

3 Mistakes That Ruin Your Patellar Tendonitis Recovery Time

Patellar Tendonitis Symptoms: 3 Red Flags You Need to Know
What is Jumper's Knee And How To Treat It | Performance Health
Patellar Tendonitis (Jumper's Knee) | Johns Hopkins Medicine

Patellar Tendonitis - The Complete Injury Guide - Vive Health

Recovery Period & Yoga Poses for Patellar Tendonitis or Jumper's Knee
Patellar Tendonitis (Jumper's knee) - Symptoms, Causes and Treatment

Patellar Tendonitis Exercises & Treatment – Enerskin
Understanding Jumper's Knee

What is Patellar Tendonitis or a Jumpers Knee? – Howard J. Luks, MD
Patellar Tendonitis (Jumpers Knee): Symptoms, Diagnosis & Treatment

Patella Tendinopathy & the 4-stage management program for 'Jumper's knee' — Rayner & Smale

Patellar tendonitis: Symptoms, treatment, and causes
Patellar Tendonitis Jumper's Knee - Everything You Need To Know - Dr. Nabil Ebraheim - YouTube
Patellar Tendon Tear - OrthoInfo - AAOS
Shockwave Therapy for Jumper's Knee (Patellar Tendinopathy/Tendinitis)

Patellar Tendonitis, Orthopedic Knee Surgeon Richmond VA

Patellar Tendinopathy surgery and treatment options – Caring Medical Florida

Patellar tendinitis - Symptoms and causes - Mayo Clinic

4 Ways to Treat Patellar Tendinitis - wikiHow Fitness

Patellar Tendinitis: How to Maximise Your Recovery – Chief Nutrition

Patellar tendonitis: Signs, symptoms and remedies for this difficult knee problem - YouTube

Quadriceps Tendonitis (Tendinopathy) - Sportsinjuryclinic.net

Patellar Tendonitis | Runner's Knee Treatment, Braces & Surgery

3 Mistakes That Ruin Your Patellar Tendonitis Recovery Time - YouTube
Patella Tendinopathy & the 4-stage management program for 'Jumper's knee' — Rayner & Smale
Jumper's Knee vs. Runner's Knee

How I Eliminated Chronic Patellar Tendonitis Once and For All
Patellar tendinopathy | Health Information | Bupa UK

Patellar Tendonitis | Treatment, Symptoms, Exercises | Airrosti

3 Exercises to Help Relieve Knee Pain | Patellar Tendonitis | Airrosti

Fixing Patellar & Quad Tendon Pain – Squat University

Patellar Tendonitis | Symptoms, treatment & recovery exercises | SportsMD

Patellar Tendonitis, Orthopedic Knee Surgeon Richmond VA

Patella Tendinopathy & the 4-stage management program for 'Jumper's knee' — Rayner & Smale

How to Fix Patellar Tendonitis (No More KNEE PAIN!) - YouTube

Patella Tendon Repair - Knee - Surgery - What We Treat - Physio.co.uk
Jumper's Knee (patellar tendonitis) Specialists Doctors | Brooklyn NYC

Osgood Schlatter Disease | Treatment, Exercises & Surgery
Posting Komentar untuk "patellar tendonitis recovery time"